Early Disease Detection: Can AI Catch What Doctors Miss?
STEM | AI & Medicine
By Aya Safa
Source: Buckhead Dermatology
Every year a staggering 11 million humans die from Sepsis – one death every 2.8 seconds.³ “It is one of the leading causes of death in the United States, on par with cancer and heart disease,” says Yale Medicine emergency physician John Sather, MD.⁹
Source: Global Sepsis Alliance
Background Information
Sepsis, a very serious condition, is the result of the body’s deadly and improper response to any type of infection an individual has, such as bacterial, fungal, or viral.⁷ This occurs because the body’s immune system has been weakened – possibly by physical trauma or burns, cancer, or diabetes – which causes molecules from the body’s immune system to attack its own tissues and organs, instead of killing bacteria and viruses.⁷ This attack results in low blood pressure, increased heart rate, and confusion.
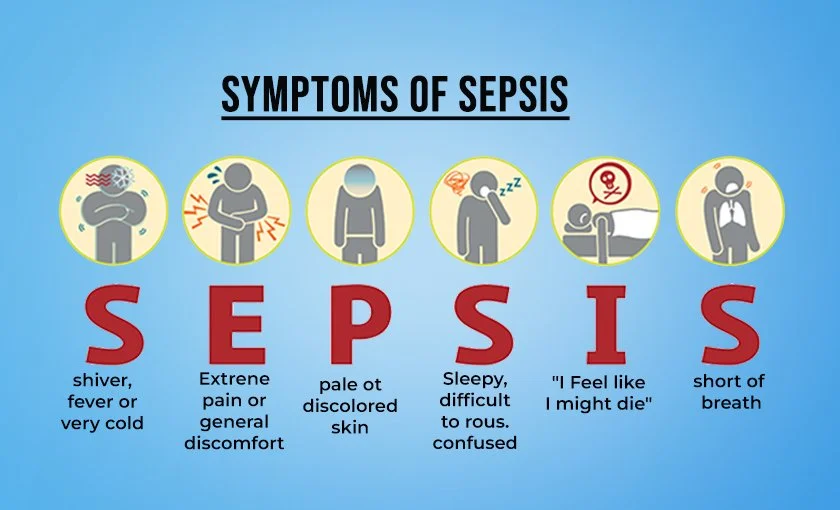
Now, many of you may be thinking what causes Sepsis to result in high mortality rates? Sepsis is extremely hard to detect because it has non-specific symptoms – chills, hypothermia, low blood pressure, rapid heartbeat – that are often misinterpreted because they're so similar to other conditions such as flu or chest infections.² Not only, but Sepsis progresses tremendously fast as one can develop “from initial infection and progress to septic shock in as little as 12 to 24 hours.”¹¹Due to these factors, there isn't an official detection system or test that determines if a patient has Sepsis.
Stages of Sepsis
Take this scenario of Mrs. Julie who spent numerous days in the Hospital due to Sepsis:
Stage One: Sepsis - First, she begins to experience certain symptoms such as mild fever, fatigue, heavy breathing, and high blood pressure.¹² Doctors run tests and the results don't indicate anything severe.
Stage Two: Severe Sepsis - This is when organ failure occurs and Mrs. Julie begins to experience symptoms of decreased urination, change in mental status, low platelet (blood clotting cells) count...¹² At this stage, she's admitted to the ICU where she receives the most extreme care with all possible treatments.
Stage Three: Septic Shock - Mrs. Julie experiences Septic Shock and all her organs fail. These symptoms are very similar to severe sepsis, accompanied with an extreme drop in her blood pressure, and, unfortunately she dies.¹² According to Mayo Clinic, about half of the patients who experience Septic Shock die.
So, if Mrs. Julie received the right care, why did she die? TIME is the most crucial aspect when it comes to treating Sepsis. The NHS emphasizes that “If sepsis is not treated early, it can turn into septic shock and cause your organs to fail. This is life threatening.”
Therefore, what led to Mrs. Julie’s death was that she was diagnosed too late which is not a surprise as “Sepsis is often missed as 50% of screening tools don’t work.” ¹
Source: KBK Hospitals
What is AI’s role in finding a solution to detecting Sepsis?
Dual Approach of Sepsis Blood Test & AI
In 2022 IntelliSep, a 10-minute laboratory blood test that uses AI and medical imaging to detect Sepsis, was approved to be marketed by the FDA. Hollis O’Neal, MD, the National Principal Investigator in this research journey, highlights that “IntelliSep is truly a game changer.”
Source: Pathology In Practice
How does IntelliSep operate?
1. Neutrophil Extracellular Trap (NET) Formation
NETs play a central role in our immune system response, specifically during infections. These structures, which are composed of DNA and neutrophil-derived proteins, trap pathogens like bacteria and fungi, which act as a defense system against infection.¹⁰ Although, in the context of Sepsis the immune system is over activated which leads to excessive NET formation.10 When this occurs, NETs will begin to attack and damage the body's tissues which ultimately leads to organ failure.¹⁰ Therefore, IntelliSep uses NETs as biomarkers to determine the probability or risk of a patient having Sepsis.
2. Extracting a blood sample from the patient
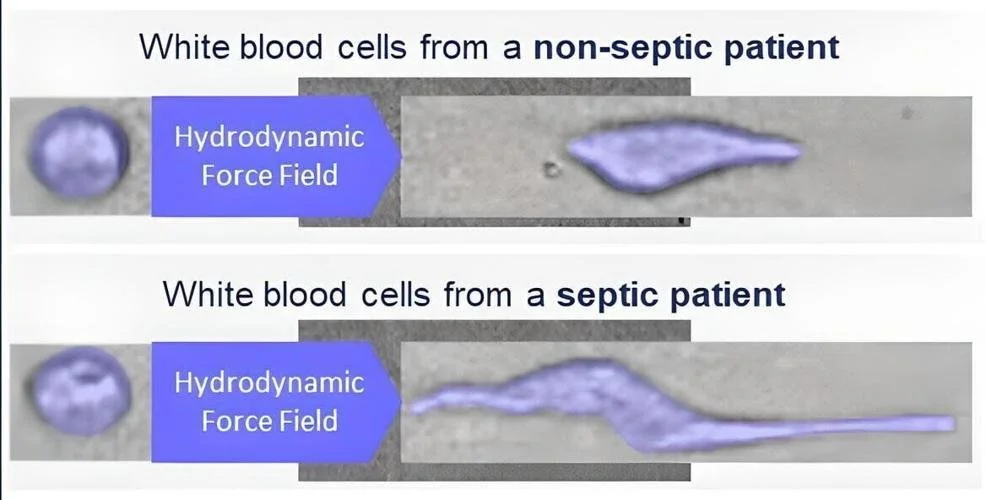
IntelliSep works by extracting blood samples from patients who exhibit Sepsis symptoms in the emergency room.⁵ White blood cells act as a marker to indicate whether the patient is positive, as individuals who carry Sepsis have softer and spongier white blood that appear elongated and compressed.⁵ For this reason, the patient’s white blood cells are squeezed through a tiny tube to identify any changes in their texture and shape.
Source: NonStopLOCAL
3. Medical Imaging & AI model
Then, a high speed camera takes images of the cells while capturing up to 500,000 frames per second.⁵ These images are then analyzed by an AI computer whose algorithm calculates the total number of elongated white blood cells.⁵ To determine the degree of risk for Sepsis in each patient, IntelliSep separates patients into three bands:
Source: Cytovale
Band One (Low risk) - The patient has a low probability of Sepsis
Band Two (Medium risk) - Further investigation and additional assessments are required
Band Three (High risk) - High probability of Sepsis and the patient receives immediate medical attention
Once the AI model determines what band the patient is a part of, physicians will be fully aware about the patient’s condition and will be able to effectively implement treatment plans. To further complete the study researchers tested 1,002 ER patients which of whom exhibited symptoms of Sepsis and the results show that IntelliSep:⁵
Accurately identified patients without sepsis with an accuracy rate of 97.5%. No deaths occurred for patients with low-risk scores.
An accuracy rate of 55% for patients who are positive for Sepsis.
This fascinating AI technology is being used in a few hospitals in Louisiana and should be implemented in 10 other hospitals by the end of 2024.⁵
COMPOSER Deep Learning AI Model
IntelliSep isn't the only method that has been produced to accurately detect Sepsis. In fact, tons of researchers around the world are trying to revolutionize the detection of Sepsis and mitigate mortality rates. In a new research study, published in January 2024 on npj Digital Medicine, researchers from UC San Diego Health System aimed to battle Sepsis by evaluating the impact of a deep learning model, COMPOSER. This AI model has been implemented in emergency departments at UC San Diego Health to predict Sepsis before symptoms became visible.⁸
Source: Medical News Observer
“Our COMPOSER model uses real-time data in order to predict sepsis before obvious clinical manifestations,” said study co-author Gabriel Wardi, MD, chief of the Division of Critical Care in the Department of Emergency Medicine at UC San Diego School of Medicine. What’s unique about COMPOSER is its ability to monitor over 150 patient variables, such as medical history, symptoms, and lab results, in order to identify the risk of Sepsis.¹⁴ If a patient presents several variables linked to Sepsis, such as low blood pressure and high temperatures, the nursing team will be notified via the hospital's electronic health record and the patient will receive rapid and extreme care.¹⁴
Results
The study analyzed data from 6,217 adult septic patients and findings reveal a 1.9% decrease in in-hospital sepsis mortality, translating to a 17% relative decrease.8 Moreover, a 5.0% increase occurred in sepsis bundle compliance, which demonstrates how COMPOSER enabled quicker interventions, and a 4% reduction in the 72-hour Sequential Organ Failure Assessment (SOFA).⁸
AI’s ability to ‘catch what doctors miss’ extends far beyond disease detection to diverse fields of healthcare such as personalized medicine, medical imaging, drug discovery, and digital health monitoring. Applications of AI to find solutions in Sepsis detection have shown incredible results, and with continued advancements and global implementation, these AI models will have the ability to further decrease mortality rates. This marks a very exciting era, not only for the healthcare community but for society as a whole as AI’s promising results are set to improve patient outcome and healthcare quality.
References
Campbell, D. (2023, September 19). Sepsis often missed as 50% of screening tools don't work, study finds. The Guardian. Retrieved October 26, 2024, from https://www.theguardian.com/society/2023/sep/19/sepsis-missed-50-percent-screening-tools-do-not-work-study-finds
Dugdale, D. C., & Conaway, B. (n.d.). Sepsis (Septicemia) – Symptoms and Causes. Penn Medicine. Retrieved October 26, 2024, from https://www.pennmedicine.org/for-patients-and-visitors/patient-information/conditions-treated-a-to-z/sepsis
Global Sepsis Alliance. (n.d.). Definition of Sepsis. Global Sepsis Alliance. Retrieved October 26, 2024, from https://globalsepsisalliance.org/sepsis
Mayo Clinic. (n.d.). Sepsis: Life-threatening complication of infection-Sepsis - Symptoms & causes. Mayo Clinic. Retrieved October 26, 2024, from https://www.mayoclinic.org/diseases-conditions/sepsis/symptoms-causes/syc-20351214
Michel, R. (2024, September 16). 10-Minute Blood Test Uses Digital Images and AI to Determine Sepsis Risk for Emergency Room Patients. Dark Daily. Retrieved October 26, 2024, from https://www.darkdaily.com/2024/09/16/10-minute-blood-test-uses-digital-images-and-ai-to-determine-sepsis-risk-for-emergency-room-patients/
National Health Service (NHS). (n.d.). Treatment and recovery from sepsis. NHS. Retrieved October 26, 2024, from https://www.nhs.uk/conditions/sepsis/treatment-and-recovery/
National Institute of General Medical Sciences. (2017, November 1). Sepsis: The body’s deadly response to infection [Video]. YouTube. Retrieved October 26, 2024, from https://www.youtube.com/watch?v=V23GXZ8fRUc
Penna, S. (2024, January 25). COMPOSER AI Model By UC San Diego Reduces Sepsis Mortality. Medical News Observer. Retrieved October 26, 2024, from https://medicalnewsobserver.com/2024/01/25/composer-ai-model-by-uc-san-diego-reduces-sepsis-mortality/
Yale Medicine. (n.d.). Sepsis > Fact Sheets. Yale Medicine. Retrieved October 26, 2024, from https://www.yalemedicine.org/conditions/sepsis
Zhu, S., Yu, Y., Qu, M., Qiu, Z., Zhang, H., Miao, C., & Guo, K. (2023, August 25). Neutrophil extracellular traps contribute to immunothrombosis formation via the STING pathway in sepsis-associated lung injury. Cell Death Discovery. Retrieved October 26, 2024, from https://www.nature.com/articles/s41420-023-01614-8
Zimlich, R. (2024, May 28). Early Signs of Sepsis: Symptoms and When to Seek Care. Verywell Health. Retrieved October 26, 2024, from https://www.verywellhealth.com/early-signs-of-sepsis-5498608
Cleveland Clinic. (2022, June 14). Septic Shock: Causes, Symptoms & Treatment. Cleveland Clinic. Retrieved October 28, 2024, from https://my.clevelandclinic.org/health/diseases/23255-septic-shock
Cytovale. (n.d.). IntelliSep Sepsis Test. Cytovale. Retrieved October 28, 2024, from https://cytovale.com/our-solution/intellisep-sepsis-test/
UCSanDiego Health. (2024, January 23). Study: AI Surveillance Tool Successfully Helps to Predict Sepsis, Saves Lives. UC San Diego Health. Retrieved October 28, 2024, from https://health.ucsd.edu/news/press-releases/2024-01-23-study-ai-surveillance-tool-successfully-helps-to-predict-sepsis-saves-lives/